meaning, goals and perspectives
It is hoped that with the concept of “tissue engineering”, namely biomimetic scaffolds, stem cells and singling molecules, pulp regeneration is an achievable goal. Αccording to its definition, regenerative endodontics aims to revitalise necrotic pulp tissue of immature permanent teeth, when necrosis is caused by infection, trauma or any developmental anomaly.
Teeth with necrotic pulp and open apexes are conventionally being treated with ‘apexification’ using calcium hydroxide to induce apical hard tissue barrier formation or MTA plug to shorten the treatment time and avoid the vulnerability of coronal restoration’s re-infection. However both techniques fail to promote vitality restoration or root maturation. Clinical researches have shown that biologically based procedures eliminate clinical symptoms of apical periodontitis, thicken canal walls and lead to apical closure in permanent immature teeth with necrotic pulp. There are two possible strategies: ‘cell transplantation’ and ‘cell homing’.
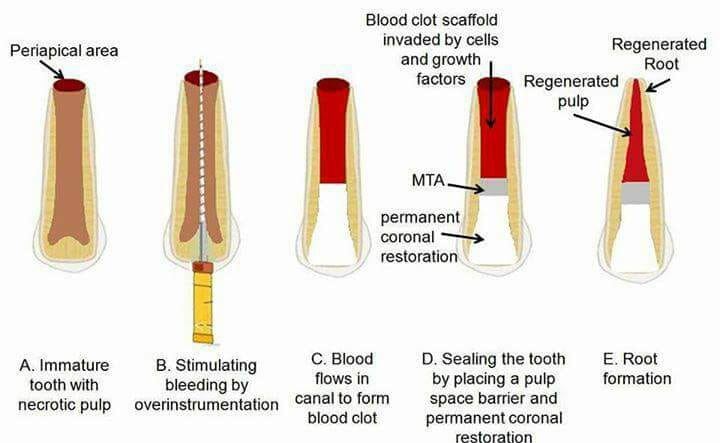
Cell transplantation means allowing regeneration through transplantation of exogenous stem cells loaded onto scaffolds with signaling molecules into the root canal system. This technique requires complex procedures, is not economically viable and has a great risk of tumorigenesis and immune injection. Many of the above challenges are circumvented by the ‘cell homing’ procedure, in which the recruitment of endogenous stem cells achieves tissue formation. Scaffols with growth factors promote angiogenesis and enhance migration. Chemotaxis occurs and leads to pulp regeneration. This process includes two steps, each one connected with an appointment, with an one week interval between them. The first step is to disinfect the root canal through irrigation. NaOCl 1,5% is bactericidal and has no toxic effects on the stem cells, whereas EDTA 17% can promote the release of GF’s located within the dental tubules. To sterilise the infected root a triple antibiotic paste is suggested comprised of minocycline, ciprofloxacin and metronidazole. Minocycline though, is thought to cause tooth staining. The use of Augmentin instead of the triple paste is clinically shown to only affect bacterial cells and thus it is widely accepted. The second step includes the induction of intra-canal bleeding, so that blood clot can act as a scaffold which will provide platelet-derived growth factors and mesenchymal cells for pulp regeneration. Alternatively, platelet-rich plasma (PRP) or platelet- rich fibrin ( PRF) could be used. These growth factor sources are said to provide improved regeneration. This can occur because periapical tissues are said to contain a higher concentration of stem cells compared to the systemic circulation. Placing PLP facilitates the migration of the periapical stem cells. The final stage would be to seal with MTA and place a permanent coronal restoration.
Follow ups are needed so as to evaluate the results; pain, soft tissue swelling and increased radiolucency indicates failure of the procedure. During the first 6-12 months we await the tooth to be asymptomatic, the walls slightly thickened and the periapical radiolucency resolved. Within 12-24 months after the treatment an increased tooth length and thickness would indicate a successful therapy.
However, the type of tissues formed are not of pulpal origin but fibrous connective tissue and cementum , likely from the periapical tissues. This probably suggests that a long-term exposure to pro-inflammatory cytokines can inhibit the dentinogenic differentiation of stem cells from the apical papilla. One of the concerns about the tissue formed is that it cannot form reparative dentine to provide protection from external insults. Although the vitality of damaged tissue is restored, the biological function as a dental pulp is lost.
All the above suggest that regenerative endodontic treatment (RET) needs further investigation. To achieve a high level of evidence there is a need for long-term and well-conducted randomized clinical trials. Extension of these advantages to healing mature teeth with pulpal necrosis would provide significant therapeutic benefits for a larger proportion of the population. These developments in regeneration of a functional pulp-dentine complex have a promising impact on efforts to retain the natural dentition.